
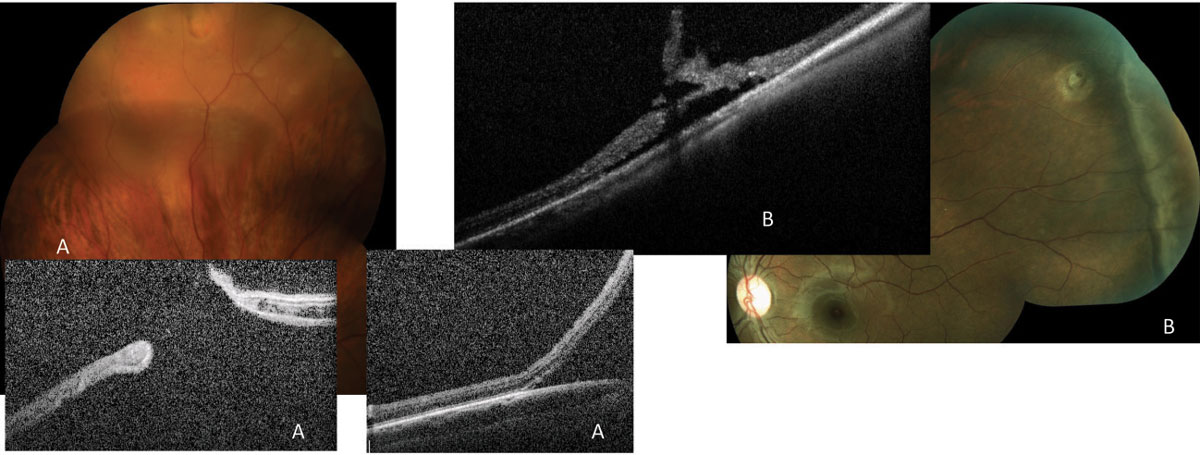
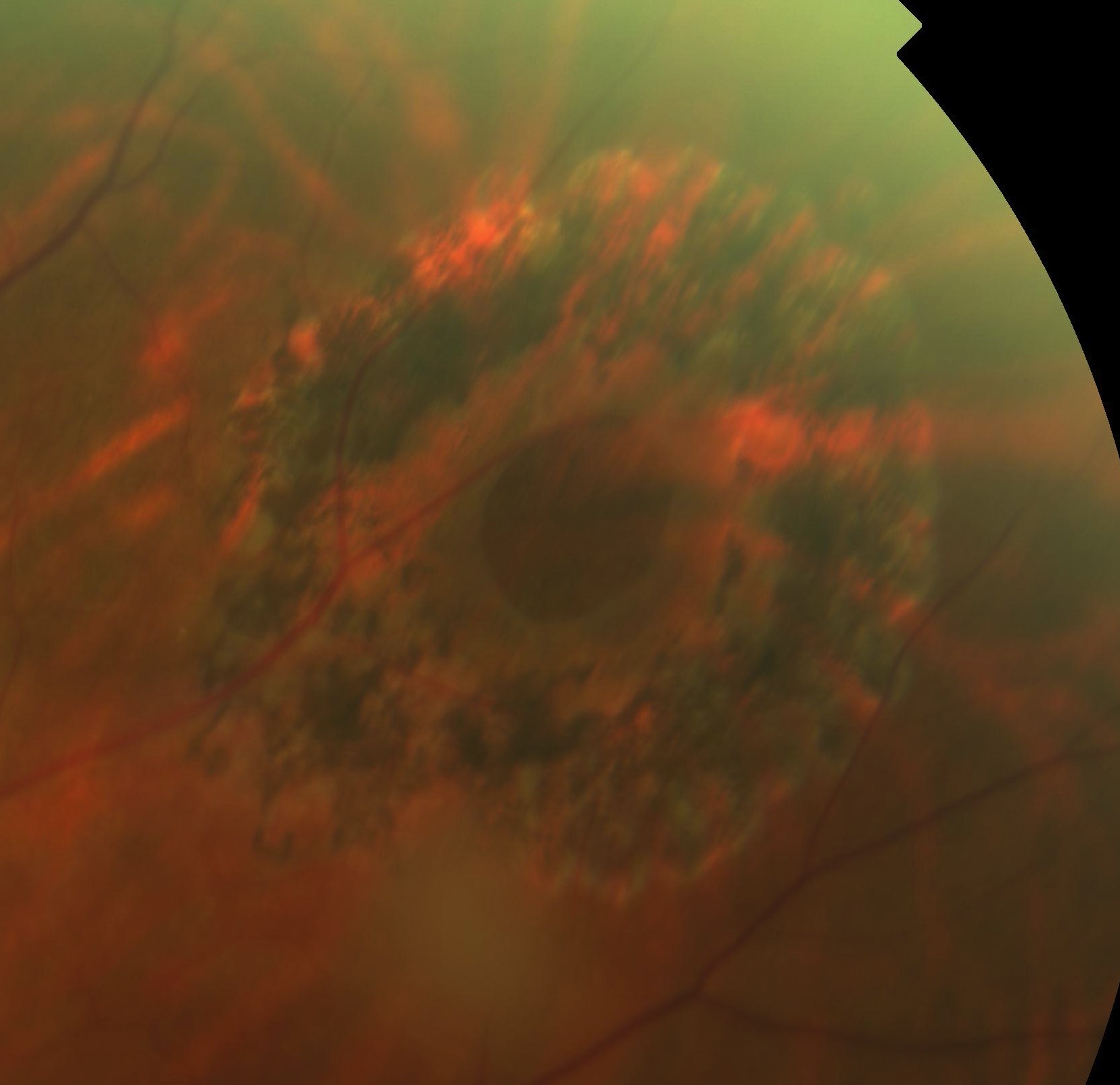
Moreover, surgical success in MH repair was found to be more than 90% within one year after the onset of the symptoms and lowered to 47.4% after 1 year. Another study reported that the rate of MH closure was only 56% in eyes with a large MH of > 400 μm and about 10% of the closed MHs reopened after 6 months. The 5-Year Manchester Large Macular Hole Study found a higher success rate between 91 and 98% of surgical closure for large MHs with diameter in the range of 400–649 μm while MHs with diameter 650–1416 μm only achieved 76%. Large MHs, MHs with a basal diameter of > 400 μm, are likely to have a flat-open closure or flat MH margins with bare RPE configuration with unsatisfactory visual prognosis despite closure. Secondary MHs are attributed to but not limited to high myopia, trauma, proliferative diabetic retinopathy, and various retinal pathologies.Ĭurrent surgical techniques successfully close majority MHs greater than 90% with remarkable visual acuity gain however, small percentages of MHs have a higher risk of initial surgical failure. Its estimated annual incidence is up to 8.69 eyes in 100, 000 population. MHs are predominantly idiopathic (primary) with higher prevalence with increasing age and in females. MH is characterized by a vertical defect in the neurosensory retinal anatomy particularly in the foveal region that extends from the internal limiting membrane (ILM) to the retinal pigment epithelium (RPE) and it affects the central vision and causes metamorphopsia. Macular holes (MHs) were once considered non-treatable and an MH was first described in 1869 from a traumatic origin. Despite relative success anatomically and visually after each technique, most techniques require a long-term study to analyze their safety profile and to establish any morphological changes of the MH plug in the closed MHs. Even in eyes with limited ILM, surgical options included autologous retinal graft, human amniotic membrane, and creation of a distal ILM flap that can assist in MH closure even though the functional outcome may be affected by the MH chronicity. In addition, several studies had shown that ILM flap manipulations in combination with surgical adjuncts increase surgical success, especially in difficult MHs. There are robust data supporting inverted ILM flap as the first-line treatment for large idiopathic MHs and certain secondary MHs including myopic MHs. A narrative review was performed on the surgical treatment of challenging MHs including large and extra-large MHs, myopic MHs with or without retinal detachment, and chronic and refractory MHs. However, a small subset of MHs imposes challenges to surgeons and frustrations on patients. Current surgical treatment for MHs is pars plana vitrectomy with epiretinal membrane, internal limiting membrane (ILM) peeling, gas endotamponade, and prone posturing postoperatively. Without successful surgery, most people lose the ability to read in the affected eye and are "legally blind" because of poor central vision.Modern surgical interventions effectively treat macular holes (MHs) more than 90%.
Fortunately, we can help you rent a chair and other equipment to assist with staying on your stomach, face down. After the surgery, face down positioning is required for a week. The jelly is replaced with a temporary gas bubble that that disappears over a few weeks. Small instruments are inserted through the white part of the eye and used to remove the jelly and relieve the traction.
#Hole in retina surgery full#
If a full hole develops, a surgical procedure called a vitrectomy is required to repair the macular hole. In some cases of vitreous traction, the jelly will separate and release from the retina, leading to spontaneous recovery. Those who have had a macular hole for less than 6 months have better chance of repair than those who have had the condition longer. Approximately 10-15% of people who develop a macular hole in one eye will develop one in the other as well. This makes reading and driving difficult and usually causes severe vision loss. Typically, people will notice a central blurry spot that progresses to form a "missing area" right in the center part of vision. While the majority of macular holes just happen on their own, severe eye trauma and other pathologic eye conditions may be related. If it does not separate cleanly, it can pull at the retina and cause traction or even a hole to develop in the very center of vision. With time, it liquefies and separates from the retina, usually occurring at age 50-60. The clear vitreous jelly fills the eye cavity and is attached to the retina from birth. Macular Holes are thought to occur from tangential traction exerted on the retina. If the retina develops a complete hole, a black "missing" spot is seen everywhere the eye looks.
The macula is the central part of the retina that is responsible for the detailed, clear vision necessary when reading or driving.


 0 kommentar(er)
0 kommentar(er)
